Type-2 Diabetes (T2D) affects over 350 million people, and current trends put that number over half a billion within 20 years.[1] Clearly this is a space where therapeutic advancements are needed to alleviate both its sufferers, and the burden that it places on national health care systems. Recent additions to the literature surrounding T2D make tremendous progress in both elucidating the molecular mechanisms of the disease,[2] and identifying an actionable therapeutic approach that could be available to patients in the near future.[3]
Our bodies use glucose as an energy currency. We take in glucose and its building blocks in our diets, and our liver can compensate for prolonged fasting by producing glucose and pumping it into our blood as needed. When our organs have enough glucose, our body produces insulin to stop glucose from being released into our bloodstream and taken up by our organs. In type-1 diabetes, the body loses the ability to manufacture insulin, but in T2D, insulin production is not a problem. Instead, peripheral tissues, like muscles, become insensitive to insulin, which is released after blood glucose increases following a meal. Ordinarily, insulin will cause the liver to drop glucose production and muscle cells to take glucose out of the blood to convert into the storage molecule glycogen. In T2D, the liver keeps right on pumping out glucose regardless of insulin levels, and muscle cells do not take up excess blood glucose. The resultant chronically elevated blood glucose levels cause a multitude of unpleasant, and potentially lethal symptoms.[4]
Obesity has long been linked to the development of T2D, and this linkage spurred much of the early research in the field to be directed at fatty acid metabolism and lipid signaling in fat, liver, and muscle – we’ll refer to these as metabolic tissues. Metabolic research has led to a vast scholarship concerning hormonal signaling, the effects of energy balance, mitochondrial dysregulation, and more.[5]
One such area that has proved crucial and spurred a huge amount of research is the relationship between metabolism and inflammation.[6] Obesity increases the levels of pro-inflammatory cytokines (cell-signaling molecules) in metabolic tissues and immune cell infiltration into those tissues, and it primes those immune cells into a pro-inflammatory state. This inflammatory state, unlike the one that occurs after infection or injury, is long-lived. It develops gradually to a constant level that scales with insulin resistance and degree of obesity, and it actually changes the compositions of metabolic tissues.[7]
The role of inflammation and the innate immune system is becoming clearer in metabolic tissues, but these inflammatory processes in the brain mostly remain mysterious. A group of researchers at Albert Einstein College of Medicine in the Bronx has just substantially expanded our knowledge in this field, focusing on the hypothalamus[2]. The hypothalamus is a small area of the brain that, along with the pituitary gland, links the nervous system to the endocrine system. The hypothalamus is involved in regulating glucose levels, and recent work had shown that it experiences inflammation in both obesity and aging; getting older increases the risk of diabetes independently of obesity. Hypothalamic inflammation is a result of an atypical activation of nuclear factor-κB (NF-κB). NF-κB is a transcription factor at the nexus of many different signaling pathways involved in both immunity and the nervous system.
All of this evidence seemed to point toward chronic inflammation acting through the hypothalamus to contribute to T2D, but some of the connections were missing. This team made the crucial insight that, in certain cell types, inflammatory signals sometimes act in a way that is the exact opposite of their typical action. Recall those cell signaling molecules called cytokines that carry inflammatory signals –the researchers examined the cytokine Transforming Growth Factor beta (TGF-β), which is well known for its roles in cell proliferation, differentiation, and immune functions. It is released in response to inflammation, and generally acts as an anti-inflammatory. However, the team at Albert Einstein showed that, in the hypothalamus, an excess of TGF-β uninhibits the transcription factor NF-κB increasing obesity- or age-related inflammation, and contributing to T2D development.
Proving this involved several steps: The scientists’ first task was to show that TGF-β levels were elevated in obese and aged individuals. They compared hypothalamic TGF-β levels in three split groups of mice: mice in one group were either fed normal chow or fed a high-fat diet. Another group was split between mice allowed to eat to their content and calorie-restricted mice. The third group was split between middle-aged and young mice. The high fat, high calorie, and aged mice all had higher hypothalamic TGF-β than their normal fat, calorie restricted, and younger counterparts.
The scientists then tested the effect of hypothalamic TGF-β on metabolism. To examine effects of hypothalamic TGF-β without including confounding diet-associated effects or body-wide TGF-β action, they fed all mice the same diet, and administered TGF-β directly to the hypothalamus. Direct administration did not raise blood TGF-β levels, thereby ruling out a systemic effect, but it did lead to both glucose intolerance and insulin intolerance in a dose-dependent manner. The scientists also showed that mice with the hypothalamic TGF-β treatment did not shut down glucose production from the liver in response to blood insulin levels. Taken together, these results suggest direct administration of TGF-β to the hypothalamus is able to recapitulate pre-diabetic symptoms in mice.
Next, the scientists sought to confirm the hypothesis that excess TGF-β in the hypothalamus acts through the transcription factor NF-κB pathway. Because NF-κB is a multi-unit protein complex, they examined the levels of each subunit in mice receiving the TGF-β injections. Most of the subunits showed no difference in abundance following injection. However, one subunit, IκBα, was found in significantly reduced levels on TGF-β treatment. This subunit holds NF-κB outside of the nucleus, where it is unable to affect gene transcription. When IκBα levels are reduced, the rest of NF-κB can move into the nucleus, and transcription begins. Thus, based on the effects it has on IκBα, excess TGF-β indeed increases the activity level of NF-κB. This result was confirmed in mice that were engineered to have only one copy of the TGF-β gene instead of the usual two copies. These mice with half the normal TGF-β did not show glucose or insulin intolerance in response to a high fat diet, despite showing the same relative increase in hypothalamic TGF-β levels. So, halving the amount of TGF-β is enough to avoid pre-diabetic symptoms on a high fat diet, as doubling TGF-β levels in these mice just brings them up to normal. These results indicated that there is a threshold level of TGF-β, above which symptoms appear.
Finally, the scientists were able to determine exactly how TGF-β regulates NF-κB activity. They showed that the increased TGF-β did not affect the usual inflammatory signaling cascade, which left unclear what causes the drop in IκBα levels that activates NF-κB. It turns out that the mRNA of IκBα contains a sequence that specifically marks it for degradation in a stress response. In response to stress, cells can sometimes sequester certain mRNAs in structures called stress granules and processing bodies. This sequestration prevents those mRNAs from being translated into protein, and eventually leads to their degradation. High-fat diet, old age, and direct injection of TGF-β all lead to an increase in the number of RNA stress granules in the hypothalamus. The scientists reintroduced IκBα into hypothalamus cells and found that this prevented NF-κB activation, and attenuated the pre-diabetic effects of excess TGF-β.
The authors sum up their results by stating, “Altogether, our findings suggest that a hypothalamic process consisting of TGF-β excess, RNA stress response and IκBα mRNA decay mediates the metabolic dysfunction that occurs during dietary obesity.” This work is a breakthrough in our understanding of how inflammation in the brain contributes to T2D, and will certainly lead to more discoveries about which signals downstream of this effect transform this stress signal into the glucose and insulin insensitivity in T2D. However, both TGF-β and NF-κB operate all over the body, and it is difficult to administer drugs to the brain, where these factors cause problems. Unfortunately, then, these results are unlikely to lead directly to useful therapeutics.
Fortunately, another recent paper from an international group including scientists from the Netherlands, the U.S.A., Australia, and China promises to do just that.[3] These researches looked at a different family of growth factors called fibroblast growth factors (FGFs). Their story starts with thiazolidinediones, a class of drugs currently used to treat insulin insensitivity by targeting a receptor that controls parts of lipid metabolism. Because of their effects on such a wide set of genes, these drugs have many unwanted side effects. The researchers thought that by targeting one of the genes downstream of this receptor, they could create a more precise tool to combat insulin insensitivity without side effects. They knew that FGF-1 is one of the genes helpfully upregulated by thiazolidinedione treatments, and that mice lacking the FGF-1 gene are more susceptible to diabetes when placed on a high fat diet.
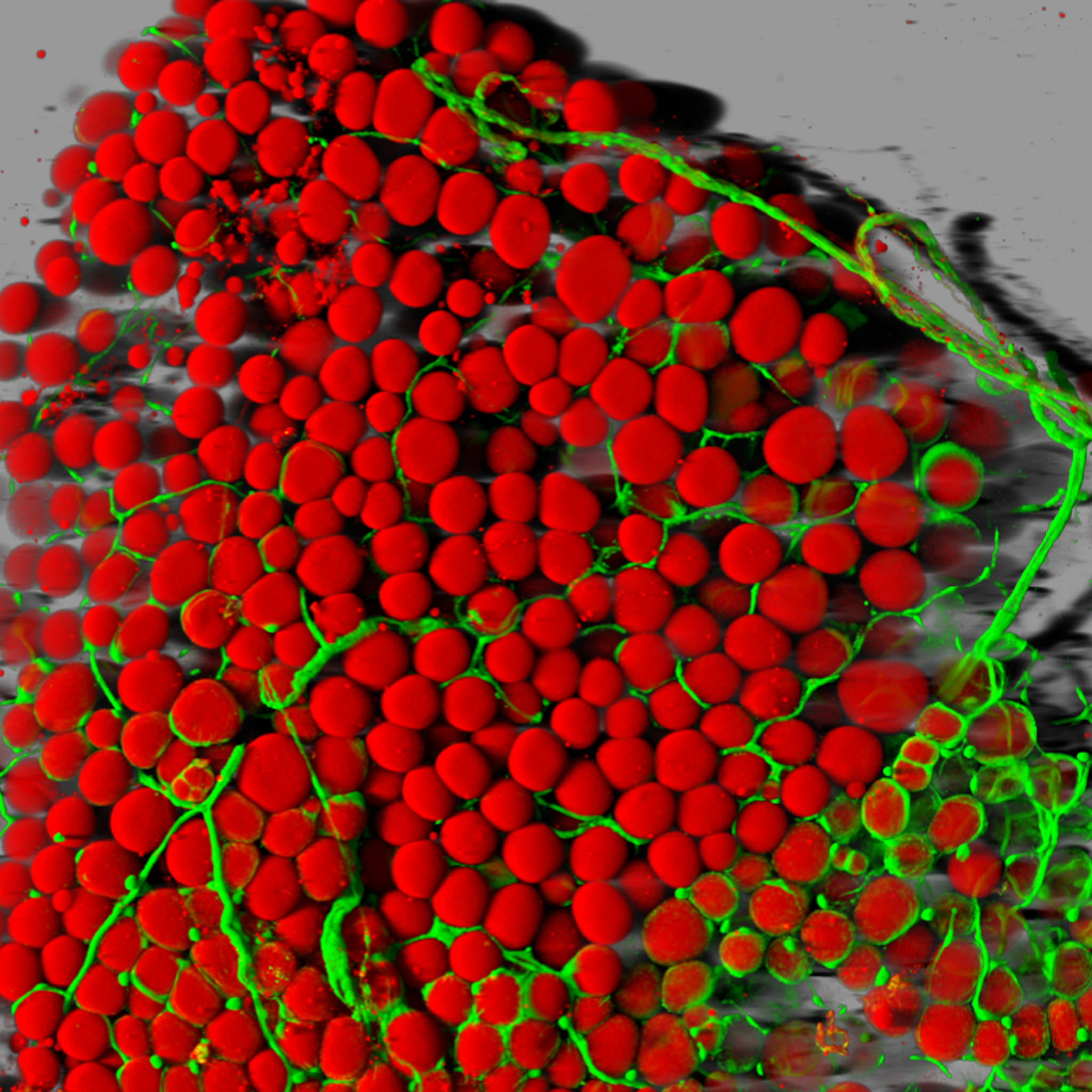
FGF-1 is what is known as an autocrine or paracrine factor. These are hormones that only affect the cell that produced them or cells nearby, respectively. This is different from an endocrine factor that enters circulation and can affect distant tissues, or even the whole body. FGF-1 has a high affinity for a part of the extracellular matrix, a gel-like network outside cells. FGF-1 gets stuck there shortly after it’s secreted and can therefore only act very near to the cell that secreted it. The idea driving this research is that we can change FGF-1 from an autocrine/paracrine factor into an endocrine factor so that it can act throughout the body to combat insulin insensitivity. Researchers injected FGF-1 into the bloodstream of both mice with genetically induced diabetes and mice with diet-induced diabetes, and in both cases the treatment reduced severely high blood sugar to normal levels. Promisingly, even high doses did not drop blood glucose below normal levels, showing that this treatment did not just drop glucose from any arbitrary starting point, but restored proper glucose regulation. This result was confirmed by application of FGF-1 to non-diabetic mice, which showed no glucose response to the treatment.
Next, concerned that the mice would develop a tolerance for repeated treatment and stop responding over time, the researchers made serial injections. During 35 days of receiving injections every other day, mice on the treatment had continually lower blood glucose levels and performed better on both glucose tolerance tests and insulin tolerance tests than control mice did. Treated mice also showed less hepatic steatosis (fatty buildup in the liver) and increased glycogen in the liver, which means that glucose secretion from the liver decreased, as in a healthy mouse. They were also able to show that FGF-1 treatment decreased levels of pro-inflammatory cytokines in the blood plasma, suggesting that this treatment may act through some of the same pathways that were discovered by the team from Albert Einstein.
Even with the evidence that FGF-1 is an effective insulin sensitizer, it would be useless as a therapeutic if it causes severe side effects. FGF-1 has well characterized mitogenic (cell proliferation) and angiogenic (blood vessel formation) properties. This should scare people who have heard these words associated with cancer growth. Luckily, a truncated form of FGF-1 shows decreased mitogenic activity. The scientists repeated their experiments with body cavity injections of this truncated form of FGF-1 and showed that the insulin sensitizing activity remained, allaying fears of FGF-1 treatment triggering the runaway cell division that causes cancer. In an unflattering comparison, thiazolidinediones, the only insulin-sensitizing treatment currently in use, can cause weight gain, liver steatosis, and bone fractures. These were the reasons that initially spurred this line of research into a more specific manner of insulin sensitization. The authors had already shown that FGF-1 treatment actually reduces hepatic steatosis, and the mice on these treatments showed somewhat decreased appetites, so the first two common side effects of thiazolidinediones are no problem with FGF-1 treatment. The researchers also showed that bone thickness, bone architecture, and bone mineral density were all unchanged by FGF-1 treatment. To further test the safety of these treatments, they looked at adipose tissue (known to respond to FGF family members) and saw no abnormalities. Additionally, the mice showed no signs of muscle damage, and had normal locomotion and oxygen utilization.
The impressive efficacy of these treatments on multiple mouse models of diabetes, plus the lack of any obvious detrimental effects make this hormone an exciting basis for potential therapies for glucose dysregulation in diabetic patients. Recombinant human FGF-1 can be faithfully expressed in E. coli (the current method for most insulin production), which means that if it proves effective in human trials, FGF-1 production can be scaled up to industrial scale easily and cheaply.
The best way for the majority of patients to manage diabetes is through proper diet and exercise to maintain a healthy weight. However, for some patients, this is impossible. Relatively recent developments such as bariatric surgery have added to the doctors’ toolbox of ways to fight what may be the most widespread disease of our generation. We may well have less invasive treatments soon that target insulin insensitivity. As we push the boundaries of our understanding of the molecular mechanisms behind T2D, that toolbox promises to expand even further.
Sources:
[1] http://www.wjgnet.com/1007-9327/full/v20/i47/17737.htm
[2] http://www.nature.com/nm/journal/v20/n9/full/nm.3616.html
[3] http://www.nature.com/nature/journal/v513/n7518/full/nature13540.html
[4] http://en.wikipedia.org/wiki/Hyperglycemia
[5] http://www.annualreviews.org/doi/pdf/10.1146/annurev-immunol-031210-101322
[6] http://www.sciencedirect.com/science/article/pii/S1550413112001374
[7] http://www.annualreviews.org/doi/pdf/10.1146/annurev.biochem.75.103004.142512
Further Reading:
http://www.sciencedirect.com/science/article/pii/S0092867412002176